Part two: biological cancer treatment and cutaneous reactions
09/08/2023
Seborrheic Dermatitis: Dermaclub’s guide to natural treatment
09/08/2023An important modern oncological strategy to defeat cancer is to block certain cellular receptors to inhibit the functions of neoplastic cells. Named targeted therapy, it targets only the specific receptors that it has been designed to block. Targeted therapy differs from chemotherapy, which instead kills all cells regardless if they are cancerous or not.
The receptor for epidermal growth factor (EGFR) is expressed on the surface of cells. The binding between EGFR and extracellular proteins stimulates the activity of intracellular protein tyrosine kinase (TK), which in turn activates cellular functions such as migration, adhesion and proliferation.
Therefore, blocking the receptor for EGFR and/or the activation of tyrosine kinase also prevents many of the most dangerous activities in tumor development which are precisely that of cell migration, adhesion and proliferation.
In recent years, the advanced pharmaceutical industry has produced numerous drugs capable of blocking EGFR or TK. These drugs have proven to be very successful in combating epithelial neoplasms and have thus become part of treatment protocols for many human cancers.
Some of these are already marketed, while others will be soon. The most widely used drug names include cetuximab (Erbitux); panitumumab (Vectibix); gefitinib (Iressa), erlotinib (Tarceva); trastuzumab (Herceptin) and iapatinib (Tyverb).
However, right from the introduction of these targeted therapy drugs, unwanted side effects including cutaneous reactions have been recorded.
This is due to the fact that the epidermis, an epithelium that rapidly renews and reproduces, becomes distressed whenever drugs capable of blocking EGFR and/or TK are administered.
Toxic side effects to the skin occur in almost all individuals undergoing these therapies and, in some cases, levels of toxicity can reach up to grades three or four, meaning that the entire treatment course must be discontinued.
These are side effects that cannot be prevented or avoided. It is therefore important that they are addressed with specific treatments to reduce any discomfort or suffering for the individual so that they can complete the full course of cancer therapy.
Part one: inhibitors on the cell membrane
The most notable cutaneous reactions due to the inhibition of EGFR are:
Papulopustular rash
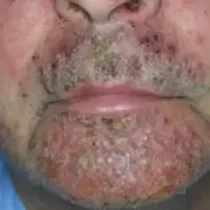
Papulopustular rash (folliculitis) is the most common side effect during treatment with EGFR inhibitors.
The reaction is characterized by the appearance of inflammatory papules or pustules at the hair follicles in locations that are especially rich in sebaceous glands, such as the face and upper trunk.
In some cases, the rash may also occur in the rest of the trunk and limbs.
In some individuals, papulopustular eruptions can be particularly intense and inflammatory plaques, due to the exuding pus from papules, form before crusting over.
Papulopustular eruptions can also appear on the eyelids and brow causing issues that are specific to that area.
When the reaction is particularly intense, eyelashes and eyebrows may fall out which may cause the individual some aesthetic concerns.
When pustules are present at the edge of the eyelid, they can discharge pus that, along with desquamation, conglomerates to form a paste that sticks to the eyelashes.
At the eyebrows, the reaction causes hair to fall out and the pooling of fluid composed of pus and dead skin cells.



Inflammation and infection of the eyelids, nasal passages and labial commissure
In certain parts of the face, such as the eyelids, nostrils and the sides of the mouth, both skin and mucosa are present. In these areas, the naturally occurring moisture provides the perfect environment in which certain bacteria and yeasts can colonize.
This can cause blepharitis (inflammation of the eyelids), nasal vestibulitis (inflammation of nasal vestibule) and angular cheilitis (inflammation of the corners of the mouth).
In addition to inflammation, cracks and/or crusts may form accompanied with sensations of burning and itchiness.



Xerosis (dry skin) and cracking
The second most common skin reaction during treatment with EGFR/TK inhibitors is xerosis cutanea, or dry skin.
Xerosis can occur anywhere on the skin area, although it is most evident on the hands and feet, and is usually the result of an impaired epidermal barrier function (EBF).
Many people mistake xerosis to be the result of a lack of water, however it is actually caused by too much water being lost from the skin due to the dysfunction of EBF.



Dry skin fissures
Cracking of the stratum corneum is a direct consequence of xerosis. Cracks as a result of dry skin can appear only the stratum corneum (superficial fissuring or fissured dermatitis), or may involve the stratum corneum and epidermis. In the latter, these cracks may lead to bleeding due to rupture of vessels in the dermis.
While cracks can occur in many locations across the body, they are usually found on fingertips where they cause burning, pain and sometimes may affect the function of the fingers.


Onychocryptosis, paronychia and reactive granulomas
Another adverse side effect that is relatively common is onychocryptosis resulting in paronychia and reactive granulomas
Onychocryptosis or, ingrown toenail, occurs when the nail plate penetrates the dermis surrounding the nail. It can occur on a single nail plate or on multiple, and can appear on the nails of both the hands and feet.
When onychocryptosis occurs, the perionychium becomes inflamed. This is referred to as paronychia and causes the distal phalanx to become red, swollen and painful whenever pressure is applied to it.
As a further consequence of onychocryptosis, a raised tissue growth named a reactive granuloma forms at the side of the nail. Reactive granulomas are painful and may appear on one or both sides of the nail.
Combined, onychocryptosis, paronychia and reactive granulomas can be so painful that they impede the ability to walk.


Changes in hair and hair growth
Unlike antiblastic cancer treatments (drugs that block cell division), targeted therapy does not usually cause hair loss.
However, hair may change in appearance and may become unrulier, thinner and more fragile.
The hairs of the eyelashes and eyebrows may undergo particularly notable changes, as they tend to grow much longer.
Eyelashes can become so long that they can disrupt vision, and may cause redness of the conjunctiva.


Photosensitivity
The targeted therapy drugs in question are not photosensitizing per se. While they do not potentiate the sun’s rays, they do make the skin unable to defend itself against ultraviolet rays.
This means that any skin that is exposed to UV rays even for a short period of time will have a more adverse reaction than usual. Symptoms of exposure include redness, swelling, itching and burning, as well as an increase in papulopustular reactions.


DermaClub’s recommended treatments
Treating papulopustular eruptions
Papulopustular rashes are categorized into four different levels, depending on their size and intensity.
A rash at level one or two does not usually require specific treatment, although additional irritation should be avoided as much as possible. Use potassium permanganate solution to cleanse the skin, before applying Soothing Cream.
Rashes that appear on the face can be particularly bothersome. They can be masked with Sun Clay, a photo-reflectant compact powder that can be applied with a brush or puff. Do not use foundation or tinted creams as their compounds can penetrate follicles which can worsen the rash. Argillina Skin Color can also be used as a natural, mineral cover-up.
As the skin is particularly dry, avoid using cleansing milk and instead remove make-up with Eudermic Cleansing Base.
Grade one or two papulopustular rash (folliculitis)
| Recommended | Avoid | |
| Soothing Cream | Cortisone | |
| Make-up | Mineral opaque
compact powder Sun Clay |
Foundation/tinted creams |
| Make-up removal | Eudermic Cleansing Base | Cleansing milks |
For papulopustular rashes of levels three or four, more targeted interventions are necessary to improve the physical condition and aesthetic appearance of the skin, and to reduce discomfort from symptoms (include redness, burning and itching).
While the rash itself cannot be prevented, symptoms such as redness, burning, itching and crusts can be soothed with 2S Cream with colloidal sulfur and salicylic acid, two naturally active ingredients that are antiseptic and anti-inflammatory. 2S Cream does not contain vaseline, which can cause further inflammation in cases of folliculitis. Apply a small amount of 2S Cream once a day to the affected area and massage well.
Do not use cortisone-based creams as they can increase the risk of infection and skin dryness. Similarly, both antibiotic-based creams and creams with retinoids should be avoided, as the former create bacterial resistance, while the latter increase dryness and inflammation.
Grade three or four papulopustular rash (folliculitis)
| Recommended | Avoid | |
| Treat with: | 2S Cream | Creams containing cortisone; antibiotics or retinoids |
| Wash with: | Eudermic Cleansing Base | Saponi, detergenti liquidi schiumogeni |
Papulopustular rash (folliculitis) treated with 2S Cream

Treating papulopustular rash on the eyelids
PEG Balm, an ointment formed with polyethylene glycols with allantoin, can be used to treat cases of papulopustular rash on the eyelids. PEG Balm absorbs secretions and helps to shed crusts. It should be applied on the outer part and not on the conjunctiva.
To clean the eyelid, do not use cleanser. Instead, cleanse with potassium permanganate solution.
Papulopustular rash (folliculitis) on the eyelids
| Recommended | Avoid | |
| Treat with | PEG Ointment | Creams containing antibiotics |
| To wash | Potassium permanganate solution | Soaps in general |
Treating the inflammation/infection of the eyelids, nostrils and labial commissure
Due to the proximity to mucous secretions such as tears, nasal mucus and saliva, the skin of the eyelids, nostrils and labial commissure is almost always moist. This moisture provides the perfect environment for the growth of bacteria and yeast, especially staphylococcus and candida albicans, respectively
Even with antibiotics and antifungals, these microorganisms are difficult to treat. However, if extreme care is taken to keep the skin as dry as possible, colonization by the microorganisms ceases spontaneously. It is therefore important that these sites should not be damped and, in order to keep clean, “dry” wash with Potassium Permanganate solution.
Potassium permanganate
Potassium permanganate (chemical formula KMnO4) is a powder that must be weighed by the pharmacist in doses of 125mg.
To make the washing solution, one liter of water is brought to boil in a pot. When water reaches boiling point, add a 125mg dose of potassium permanganate. After one minute of boiling, the powder will have dissolved and the solution is ready. Once the solution has cooled, decant into dark glass bottles (such those used for wine or oil), clearly labeled as “disinfectant.”
The solution will remain active for one month.
How to “dry” wash
To maintain body hygiene without bathing, showering and/or using detergent, the following “dry” washing routine should be adopted:
- take a cotton towel that is at least the size of a pillowcase
- place the towel at the bottom of the sink
- wet it with the potassium permanganate solution
- wring out the cotton cloth completely
- with the damp towel, massage the hair first before continuing to the rest of the body
- do not rinse; blot any residual moisture with a towel and dress as normal
- Wash once per day following the above routine.
“Dry” washing allows the individual to maintain excellent body hygiene without wetting the skin or using harsh soaps, thus avoiding any additional inflammation.
The use of antibiotic or antimycotic creams could create resistance in microorganisms. Instead, apply PEG Ointment, which absorbs exudates to dry the skin and prevent the growth of microorganisms.
Inflammation and infection of the eyelids, nasal passages and labial commissure
| Recommended | Avoid | |
| To treat | PEG Ointment | Creams containing antibiotics |
| To wash | Potassium permanganate solution | Soaps in general |
Treating xerosis (dry skin)
Xerosis (dry skin) is the result of a deficiency of epidermal barrier function during EGFR/TK inhibitor treatment. It is accompanied by itching, burning and intense desquamation, and is the precursor for cracks and fissures to appear.
The first step in overcoming dry skin is to stop washing with soaps and synthetic detergents. Washing strips some of the skin’s protective fats, which worsens dryness and its symptoms.
To wash the body, hair or hands, use Eudermic Cleansing Base. Formulated as a liquid cream, it does not foam and cleanses without drying out the skin.
After washing areas of particular dryness, apply a self-hydrating ointment. Extreme Emollient Ointment is a compound based on polyglycerides and synthetic paraffins that draws up water from deep within the skin to the surface and helps maintain it there, hence the name “self-hydrating”. If the skin dryness is not particularly excessive, use Nourishing Cream instead.
Avoid the use of moisturizing creams, which are not effective in this type of dryness and are often not tolerated by the skin.
Xerosis (dry skin) and cracking
| Recommended | Avoid | |
| To wash | Eudermic Cleansing Base | Soaps, gels |
| After washing | Extreme Emollient Ointment Nourishing Cream |
Hydrating creams |
Treating cracks and rhagades
The xerosis caused by treatment with EGFR/TK inhibitors can often cause painful and/or bleeding cracks or rhagades to form. Should this be the case, any cracks or rhagades must be kept completely dry and any contact with water should be suspended. To clean and disinfect the area affected by cracks, use Potassium Permanganate solution. After cleaning, apply PEG Ointment to protect and heal.
Avoid contact with water and soaps/detergents until healing is complete.
Cracks and rhagades
| Recommended | Avoid | |
| To treat | PEG Ointment | Antibiotics/cortisone |
| To wash | Potassium permanganate solution | Soaps in general |
Treating onychocryptosis, paronychia and reactive granulomas
Treatment of onychocryptosis (ingrown nail) often consists of removing the portion of the ingrown lamina and granuloma under local anesthesia. The corresponding portion of the nail matrix is then destroyed by phenol. With the correct care post-operation, onychocryptosis and reactive granuloma will go into remission.
The purpose of post-operative care should be to lower the local bacterial load and to reduce the pyogenic reactive granuloma. For this purpose, Astringent Gel with aluminum chloride is used. Aluminum chloride has powerful antibacterial properties and reduces granuloma by coagulating and precipitating cell surface proteins.
Astringent Gel should be massaged into the affected area two or more times a day. Although the application of Astringent Gel may cause sensations of burning that could be uncomfortable, this will stop after a few minutes. Do not cover the nail after application and do not get the ingrown toenail wet during treatment. Instead, wash the toe with Potassium Permanganate solution. To do so, apply the solution to a cotton cloth, wring out and apply to the inflamed area.
| Recommended | Avoid | |
| To treat | Astringent gel | Antibiotics/cortisone |
| To wash | Potassium Permanganate solution | Soaps in general |
Sun protection
| Recommended | Avoid | |
| Sun protection | Hat, sunglasses, Sun Clay | Suncream |
During cancer treatment with EGFR/TK blockade, it is important to avoid direct sun exposure and to suspend the use of UV lamps (sunbeds etc.)
Even with precautions, in the summer months sunlight hits any exposed parts of skin with a high UV charge, with the skin on the face being particularly vulnerable. While many think this problem could be resolved by the filters contained in sunscreen, these are particularly complex and often poorly tolerated even on healthy skin. They are, therefore, not recommended as sun protection.
Instead, to minimize UV exposure:
- Avoid the sun as much as possible.
- Always wear a brimmed hat that shades the face and sunglasses with anti-UV lenses.
- Before sun exposure, apply the photo-reflective Sun Clay to any exposed parts of the skin. Applied with a puff, it maintains its protectiveness and does not absorb into the follicles, making it the ideal protection for dermatitis-prone skin.
Make-up
| Recommended | Avoid | |
| Make-up | Sun Clay Argillina Skin Color |
Foundation or tinted creams |
| Make-up remover | Eudermic Cleansing Base | Cleansing milks |
During cancer treatment with EGFR/TK inhibitors, papulopustular reactions (folliculitis) most commonly appear on the face. In addition to the physical irritation caused by itchy, burning skin, there is also an understandable aesthetic concern.
Many may think that the best way to resolve this is to apply foundation or tinted cream to mask the lesions. However, these are greasy products (even those that claim to be oil-free) that can easily penetrate inside the follicles already inflamed by folliculitis, worsening, sometimes severely, the condition.
To mask lesions, use Sun Clay, which is made of powdered natural pigments that can be applied with a brush or puffs. For those who prefer cream make-up, use Argillina Skin Color instead of foundation. Argillina Skin Color can be used on pathological skin conditions.
To remove make-up, use Eudermic Cleansing Base. Do not use cleansing milk or similar products, as these often contain vaseline or harsh cleansers such as sodium lauryl sulfate (SLS).
References
Clinical management of cutaneous toxicity of anti-EGFR agents The International Journal of Biological Markers, Vol. 22 no. 1 (suppl 4), 2007, pp. S53-S61 2007 Wichtig Editore