
Warts: how to recognise and treat them
07/08/2023
Skin ulcers: DermaClub’s treatment options
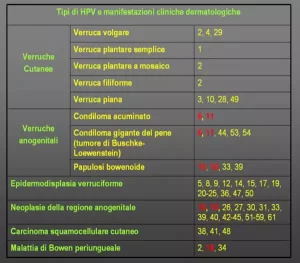
08/08/2023The human papilloma virus (HPV) is a very small DNA virus, with a diameter of around 55nm. It can penetrate the skin and mucous membrane cells, before integrating into the DNA of human cells which may cause the growth of both benign and malignant tumors. There are nearly 200 documented genetic types of HPV, the most dangerous of which are strains 6 and 11 that cause genital warts, and strains 16 and 18 that cause cervical cancer. While HPV strains cause different infections and pathologies, it is possible for more than one strain of the virus to be present in an infection. The following table shows diseases caused by HPV and the respective HPV strains that cause them.
Marked in red are viral types 6, 11, 16, and 18, which are the strains towards which the quadrivalent HPV vaccine is targeted.
Genital warts
HPV viruses also cause genital warts, or condylomas.
Genital warts are caused by HPV strains 6 and 11, and are particularly serious due to their high contagiousness and the speed at which they proliferate. Genital warts are characterized by multiple warty growths in the genital area.
In males, genital warts affect the glans and foreskin, the skin of the shaft and sometimes the pubic as well as the perianal areas.
In females, visible genital warts will appear on either the vulva or perivulvar areas, while those that appear on the vagina and cervix will only be noticed upon gynecological examination.
Viral genital warts are primarily transmitted through sexual intercourse although transmission through clothing, secretions, and objects is possible. If genital warts are caused by HPV strains 16 and 18 – instead of 6 and 11 – these can cause the degeneration of the cervix leading to cervical cancer.
Cervical cancer: HPV at its worst
The degeneration of the cervix and cervical cancer occur silently and insidiously, without any particular symptoms.
It starts with the penetration of HPV into the mucosa which, over time, causes some cells to become infected with the virus and turn cancerous.
After a few years have passed, the number of cancerous cells will have increased and invaded the entire mucosa.
If action is not taken in time, the cancer cells will slowly invade the underlying tissues and spread, at which point the tumor is uncontrollable.
HPV and carcinomas
Thanks to the relatively recent possibility to detect the presence of HPV in cells through molecular techniques, dangerous HPV strains including 16 and 18 have been linked to cancers of the oral cavity, tongue, larynx, skin and others.
With skin cancer, it is now believed that the presence of HPV in the epidermis cells, combined with UV ray exposure, is the cause of squamous cell epithelioma.
Treating genital warts
There is no specific anti-HPV drug available and therefore alternative methods must be used to treat these viral genital warts.
The proposed treatments for genital warts can be grouped into:
- thermal destructive methods
- chemical destructive methods
- “immunological” methods
Thermal destructive methods are the most common way of treating genital warts. They eliminate warts with thermal energy generated through diathermocoagulation, laser therapy and other techniques. Thermal destructive treatment is usually performed under local anesthetic and may cause several drawbacks such as slow healing of the treated areas, the possibility of infection, recurrence of genital warts, and scarring from thermal burn.Thermal destructive methods also include cold treatment or cryotherapy, however, these do not usually give good results for genital warts and are not recommended. Chemical destructive methods are mainly carried out with podophyllin or derivatives.
Podophyllin is a resin that is extracted from the rhizomes of plants belonging to the podophyllum genus and acts as an anticancer agent by blocking cell mitosis. In practice, 30% podophyllin in vaseline is used, an ointment of which must be prepared by a pharmacist. The ointment is applied over any external genital warts (not in the vagina) and left for six hours before being thoroughly rinsed. Application is repeated over three days until the genital warts have disappeared.
Podophyllin is extracted from podophyllotoxin which is the active ingredient, however as it is a very active compound, any treatment course containing podophyllotoxin must be followed according to doctor’s instructions.
“Immunological” methods involve locally stimulating an immunological response that can, in turn, eliminate genital warts.
The drug imiquimod in cream form is normally used and is able to stimulate lymphocytes to recognize and eliminate HPV-infected cells.
Unless otherwise directed by a doctor, imiquimod is applied for six to eight hours, three times a week for up to eight weeks. Genital warts are positively treated in about 60% of cases.
Photodynamic therapy has also been used in the treatment of genital warts by stimulating an immune response, but the positive results obtained are still under verification.
The HPV quadrivalent vaccine (strains 6, 11, 16 and 18)
Using genetic engineering techniques, a particle similar to the HPV virus, but without infectious DNA, has been constructed. This particle is coated with the L1 protein, which is present on HPV strains 6, 11, 16 and 18. When these particles are injected through the vaccine, the body develops specific antibodies against HPV and its four most dangerous strains. These antibodies are called neutralizing antibodies because they prevent HPV from penetrating cells and, therefore, reduce the risk of contracting diseases caused by HPV.




